Support - It’s About Time!

|
|||
| site search by freefind |
Message Boards
Documents
Download these documents. Some are in PDF format and may require the use of Adobe Acrobat. Click any of the headers to re-sort.
| Format | Title (Click to Sort) |
Description | Last Updated (Click to Sort) |
|---|---|---|---|
Excel |
Cushings Help Organization, Inc. Medical Journal |
Download Cushings Help Organization, Inc. Medical JournalKeep records of questions and answers for medical appointments, allergies, meds, surgeries and more |
3/25/2007 |
Excel |
Cortisol Test Results |
Download Cortisol Test Results
|
9/22/2007 |
iPod / Quicktime |
Interview with MaryO, Cushings-Help.com founder.(iPod / Quicktime) |
Click to ListenSubscribe on iTunes
Intro: Hello, I have with us today Mary O'Connor, founder of the cushings dash help dot com website. Mary is a 20 plus year survivor of Cushing's Disease. For those who do not know what Cushing's Disease is, you may want to peruse the Cushings-help website. Briefly, it is an endocrine-related disease caused by a pituitary tumor (also called an adenoma) which causes life-threatening symptoms. Cushing's Syndrome is a similar disease caused by an adrenal or other tumor. MaryO, as she is fondly called by the members of the support board she runs in conjunction with the website, has been instrumental in educating thousands of people about Cushing's. Through the use of her website and support boards, these same folks have been able to garner support and information invaluable to their diagnosis and treatment. She has been recognized in Forbes Magazine, many newspaper and journal articles, and is a speaker at Cushing's Awareness events. She is married to Tom and has a grown son, Michael. Mary, I know the listeners would love to hear your story. What can you tell us about your symptoms , diagnosis, and treatment with Cushing's? Other Topics Discussed:
Closing: As you can see, Mary is a survivor. Not only has she survived, but she has enabled so many others of us to survive, also. Please stay tuned for more stories from these survivors! For more information, visit the cushings-help website. Keywords: adenoma, adrenal, arginine, arthritis, aspirin, awareness, cortef, cortisone, cortrosyn, Cushing's, diagnosis, endocrine, energy, Forbes Magazine, gland, growth hormone, gym, insurance, kidney cancer, MaryO, menopause, migraine, nap, NIH, obesity, pituitary, Power Surge, rare, renal cell carcinoma, staticnrg, steroid, stimulation, support board, surgery, survivor, symptoms, thyroid, tired, transphenoidal hyposection, treatment, tumor, website, weight, Weight Watchers |
1/3/2008
|
iPod / Quicktime |
Diurnal variation in diagnosing Cushing's.(iPod / Quicktime) |
Click to Listen or Right-Click to DownloadSubscribe on iTunes
Robin says "If you have pseudo-Cushing's, this variation doesn't happen. A typical/normal person has their highest cortisol around 8 a.m. and it goes down incrementally until it is around zero at midnight. This is true of a person with pseudo Cushing's, too. A person with Cushing's Disease/Syndrome will have the variation shown in the link above. It's important to have this measured. The easiest way to find out is to have late-night serum cortisol measurements (around 11 p.m.) to see what it is at that time of night. If you have elevated late-night cortisols, it indicates Cushing's Syndrome/Disease. One test in the a.m. will not tell you enough information. Stress affects everyone's cortisol. But elevated cortisol over a period of time is due to something other than "stress". And it hurts your body. Even it is intermittent (cyclical), it is very damaging, but harder to diagnose. I hope you will go for more testing. I believe you need to find a doctor who will test 8 a.m. cortisol levels and late-night cortisol levels, preferably by both salivary and serum tests. Also, high Urinary Free Cortisol (UFC) levels are the "gold-standard" for Cushing's and if high, are very indicative. However, many of us don't have high UFC's but do have high salivary and serum levels. You need MUCH more testing to determine if you have Cushing's and to determine if your diurnal rhythm is out-of-whack!" Keywords: Cushing's, cushing, Diurnal, cyclic, rhythm, salivary, circadian, pituitary, adrenal |
12/31/2007
|
iPod / Quicktime |
Pituitary Cushing's(iPod / Quicktime version [38 MB]) |
Download Pituitary Cushing'sKate and Dr. Ted Friedman on National Geographic TV Kate (Fairley on the boards) and her doctor Dr. Ted Friedman, were featured on the National Geographic channel. The show, called the Science of Obesity, has a segment on Cushing's syndrome. Today, 127 million adult Americans are considered overweight, but few reach the extreme proportions of the exceptionally obese. What are the physical stresses of weighing more than 500 pounds and what steps can reverse it? NGC provides an understanding of what happens inside the bodies of these massive people & why a person can pack on hundreds more pounds than those with typical weight challenges. The show explores the genetics behind weight gain & medical advances available to help prevent it. I hope that all of you can watch this. Please consider contacting your local media about doing your story! There is still much work to do to increase Cushing's awareness. Robin submitted the Cushing's segment for us... |
9/19/2007 |
iPod / Quicktime |
Pituitary Cushing's(iPod / Quicktime version [38 MB]) |
Download Pituitary Cushing'sFrom
http://www.49abcnews.com/news/2006/jul/22/ Surgery could cure rare Cushing's diseaseStory by Jessica Lovell (Contact) 9:15 p.m. Saturday, July 22, 2006 This video requires the free QuickTime 7 plug-in. Download: Cushing's disease brought four women together for what they fondly refer to as their “Cushie Party.” “I don’t know about you guys, but my family didn’t even believe me,” Jaimie Augustine***, Cushing's patient, said. “You don’t gain 70 pounds in 7 months and have something not be wrong.” Cushing's disease is caused by a rare tumor in the pituitary gland. The tumor itself is not the problem, but it causes the body to produce too much of the hormone cortisol. It’s the excess cortisol that wreaks havoc on the body. “I started having hair growth on my chin, and on my arms,” Augustine said. “I got purple stretch marks on my stomach.” It didn’t matter if Augustine ate as little as a thousand calories a day, she still gained 100 pounds. It took five years before Jaimie’s doctors pieced together her symptoms and treated her for Cushing's. “Most centers that deal with this would accept that the first line of treatment is pituitary surgery, brain surgery,” Dr. William Ludlam, endocrinologist, said. During surgery, doctors remove the tumor on the pituitary gland. “It’s still actually a difficult surgery, because these tumors are typically very liquidy, soft tumors and can ooze and go places,” Dr. Ludlam said. Augustine’s surgery was a success, and she began to lose weight after doctors removed the tumor. While Augustine said she can’t wait to have her body back, she admitted Cushing's gave her a different perspective on life. More Information Dr. Ludlam cautions that pituitary surgery works dramatically for some patients, but not for all. If you have Cushing's, or think you have symptoms, you can find out more information on the disease, or find support near you. *** Message Board Members. The person sitting next to Jaimie against the head board is Kristin (lookingforanswers), Amy (kalimae) is the blonde and the one in the yellow top is Krystine. |
7/22/2006 |
Parts of the Brain |
Download Parts of the BrainGina writes "I found an excellent, simple teaching guide that's a few pages long, but diagrams all the parts of the brain in different views that you'd see on an MRI. This will show you the specific structure of the pituitary, sella, stalk, etc look like, plus lots more." |
7/1/2008 | |
Cushing's syndrome in women with polycystic ovaries and hyperandrogenism |
Download Cushing's syndrome in women with polycystic ovaries and hyperandrogenismA 41-year-old woman presented to an endocrinology–gynecology clinic having been diagnosed 7 years earlier with polycystic ovarian syndrome on account of hirsutism, subfertility, greasy skin, acne and multiple ovarian cysts. Ovulation induction had led to a successful pregnancy. Subfertility recurred, however, and persisted alongside a new diagnosis of hypertension and progressive weight gain. Upon examination, the patient was hypertensive with facial plethora, rounded facies and violaceous abdominal striae... |
5/8/2008 | |
Patient Guide to the Diagnosis of Cushing's Syndrome |
Download Patient Guide to the Diagnosis of Cushing's SyndromeSeveral factors influence the choice of the best initial test. For pregnant women, the Guidelines recommend for the use of the UFC and against the use of the DST. For patients receiving medications used for seizure disorders, (such as phenytoin, phenobarbitone, and carbamezepine), the Guidelines recommend against the use of dexamethasone, which might give false positive results. Instead, they recommend measurements of UFC or late-night blood or salivary cortisol. For patients with kidney failure, the Guidelines suggest using the 1-mg overnight DST rather than UFC. In patients suspected of having mild CS due to an adrenal mass, the Guidelines suggest use of the 1-mg DST or late-night salivary cortisol test rather than UFC. |
5/8/2008 | |
Steroid hormone flow chart |
Download Steroid hormone flow chartGreat steroid hormone flow chart, Makes it very easy to understand how they're made. Posted by Susan F (MCF). |
3/21/2008 | |
Cushing's syndrome in women with polycystic ovaries and hyperandrogenism |
Download Cushing's syndrome in women with polycystic ovaries and hyperandrogenismA 41-year-old woman presented to an endocrinology–gynecology clinic having been diagnosed 7 years earlier with polycystic ovarian syndrome on account of hirsutism, subfertility, greasy skin, acne and multiple ovarian cysts. Ovulation induction had led to a successful pregnancy. Subfertility recurred, however, and persisted alongside a new diagnosis of hypertension and progressive weight gain. Upon examination, the patient was hypertensive with facial plethora, rounded facies and violaceous abdominal striae... |
11/28/2007 | |
Diagnosis and Complications of Cushing's Syndrome: A Consensus Statement |
Download Diagnosis and Complications of Cushing's Syndrome: A Consensus StatementDiagnosis and Complications of Cushing's Syndrome: A Consensus Statement G. Arnaldi, A. Angeli, A. B. Atkinson, X. Bertagna, F. Cavagnini, G. P. Chrousos, G. A. Fava, J. W. Findling, R. C. Gaillard, A. B. Grossman, B. Kola, A. Lacroix, T. Mancini, F. Mantero, J. Newell-Price, L. K. Nieman, N. Sonino, M. L. Vance, A. Giustina and M. Boscaro Division of Endocrinology (G.A., B.K., T.M., M.B.), Department of Internal Medicine, University of Ancona, 60100 Ancona, Italy; Division of Internal Medicine (A.A.), Department of Clinical and Biological Science, University of Torino, 10063 Torino, Italy; Regional Centre for Endocrinology and Diabetes (A.B.A.), Royal Victoria Hospital and Queen’s University, BT126BA Belfast, United Kingdom; Department of Endocrinology (X.B.), University Renè Descartes and Institut Cochin, Institut National de la Santé et de la Recherche Médicale U567 and Faculty Cochin, 75014 Paris, France; Department of Endocrinology (F.C.), San Luca Hospital, Italian Auxological Institute, Instituto di Ricovero e Cura a Carattere Scientifico, University of Milan, 20149 Milan, Italy; National Institute of Child Health and Human Development, National Institutes of Health (G.P.C., L.K.N.), Bethesda, Maryland 20892-1583; Department of Psychology (G.A.F.), University of Bologna, 40127 Bologna, Italy; Endocrine-Diabetes Center (J.W.F.), St. Luke’s Medical Center, Milwaukee, Wisconsin 53215; Division of Endocrinology, Diabetology, and Metabolism (R.C.G.), University Hospital, Centre Hospitalier Universitaire Vandois, CH-1011 Lausanne, Switzerland; Department of Endocrinology (A.B.G.), St. Bartholomew’s Hospital, London EC1A 7BE, United Kingdom; Department of Medicine (A.L.), Centre hospitalier de l’Université de Montréal, H2W1T7 Montréal, Canada; Division of Endocrinology (F.M.), Department of Medical and Surgical Sciences, University of Padova, 35128 Padova, Italy; Division of Clinical Sciences (J.N.-P.), Sheffield University, Northern General Hospital, 557AU Sheffield, United Kingdom; Department of Statistical Sciences and Department of Mental Health (N.S.), University of Padova, 35128 Padova, Italy; University of Virginia Health System (M.L.V.), Charlottesville, Virginia 22908-0746; and Department of Internal Medicine/Endocrine Section (A.G.), University of Brescia, 25125 Brescia, Italy Address all correspondence and requests for reprints to: Dr. Giorgio Arnaldi, Clinica di Endocrinologia Azienda Ospedaliera Umberto I, Sede Torrette 60100 Ancona, Italia. E-mail: g.arnaldi@aoumbertoprimo.marche.it. In October 2002, a workshop was held in Ancona, Italy, to reach a Consensus on the management of Cushing's syndrome. The workshop was organized by the University of Ancona and sponsored by the Pituitary Society, the European Neuroendocrine Association, and the Italian Society of Endocrinology. Invited international participants included almost 50 leading endocrinologists with specific expertise in the management of Cushing's syndrome. The consensus statement on diagnostic criteria and the diagnosis and treatment of complications of this syndrome reached at the workshop is hereby summarized. Participants in the Consensus Workshop were: B. Ambrosi, A. Angeli, G. Arnaldi, E. Arvat, A. B. Atkinson, X. Bertagna, M. Boscaro, F. Casanueva, F. Cavagnini, G. P. Chrousos, R. N. Clayton, A. Colao, Y. de Keyzer, W. de Herder, G. Faglia, F. Fallo, G. A. Fava, J. W. Findling, R. C. Gaillard, M. Gasperi, A. Giustina, A. B. Grossman, B. Kola, A. Lacroix, A. Lania, R. Lauro, P. Loli, M. Losa, T. Mancini, M. Mannelli, F. Mantero, J. Newell-Price, L. K. Nieman, R. Pasquali, F. Pecori Giraldi, R. Pivonello, M. Reincke, F. Santeusanio, M. T. Sartori, N. Sonino, G. K. Stalla, M. Terzolo, S. Tsagarakis, M. L. Vance, and R. Vettor. Abbreviations: BIPSS, Bilateral IPS sampling; BMD, bone mineral density; CBG, corticosteroid-binding globulin; CD, Cushing's disease; CS, Cushing's syndrome; CT, computed tomography; DEXA, dual energy x-ray absorptiometry; DST, dexamethasone suppression test(s); IPS, inferior petrosal sinus; MRI, magnetic resonance imaging; UFC, urinary free cortisol. From The Journal of Clinical Endocrinology & Metabolism Vol. 88, No. 12 5593-5602 at http://jcem.endojournals.org/cgi/content/abstract/88/12/5593 |
11/16/2007 | |
Adrenal Fatigue and Cortisol-101 |
Download Adrenal Fatigue and Cortisol-101Steven F. Hotze, M.D. began to notice that many women had other health problems besides their allergies. As he listened to his patients he began to detect a pattern. Many of these women had been suffering chronic illnesses many of them due to hormonal changes, such as childbirth or midlife. Others were suffering from recurrent yeast overgrowth, thyroid disorders, adrenal fatigue, and vitamin deficiency. From Steven F. Hotze, M.D.'s Website at http://www.drhotze.com/EN/ |
11/16/2007 | |
Brain atrophy and cognitive deficits in Cushing's disease |
Download Brain atrophy and cognitive deficits in Cushing's diseaseChirag G. Patil, M.D., Shivanand P. Lad, M.D., Ph.D., Laurence Katznelson, M.D., and Edward R. Laws Jr., M.D. Abbreviations used in this paper: EAA = excitatory amino acid; LTP = long-term potentiation. Address correspondence to: Chirag G. Patil, M.D., Department of Neurosurgery, Stanford University Hospital, 300 Pasteur Drive, Room R281, MC5327, Stanford, California 94305. Email: chirag-patil@gmail.com. Abstract: Cushing's disease is associated with brain atrophy and cognitive deficits. Excess glucocorticoids cause retraction and simplification of dendrites in the hippocampus, and this morphological change probably accounts for the hippocampal volume loss. Mechanisms by which glucocorticoids affect the brain include decreased neurogenesis and synthesis of neurotrophic factors, impaired glucose utilization, and increased actions of excitatory amino acids. In this review, the timing, pathology, and pathophysiology of the brain atrophy in Cushing's disease are discussed. The correlation of atrophy with cognitive deficits and its reversibility is also reviewed. Keywords: brain atrophy; Cushing's disease; cognitive impairment; glucocorticoids; hippocampal atrophy. From The Journal of Neurosurgery, September 2007 Volume 23, Number 3 at http://thejns.org/toc/foc/23/3?cookieSet=1 |
10/31/2007 | |
Current state of the art in the diagnosis and surgical treatment of Cushing disease: early experience with a purely endoscopic endonasal technique |
Current state of the art in the diagnosis and surgical treatment of Cushing disease: early experience with a purely endoscopic endonasal techniqueAmir R. Dehdashti, M.D. and Fred Gentili, M.D., F.R.C.S.C. Abbreviations used in this paper: ACTH = adrenocorticotropin hormone; CSF = cerebrospinal fluid; FSH = follicle-stimulating hormone; GTR = gross-total resection; IGF-1 = insulin-like growth factor–1; IPSS = inferior petrosal sinus sampling; LH = luteinizing hormone; MR = magnetic resonance; TSH = thyroid-stimulating hormone; UFC = urinary free cortisol. Address correspondence to: Amir R. Dehdashti, M.D., Division of Neurosurgery, Toronto Western Hospital, Fourth Floor, West Wing, 399 Bathurst Street, M5T 2S8, Toronto, Ontario, Canada. email: amirdehdashti@hotmail.com. Object: Transsphenoidal pituitary surgery is the primary therapy for Cushing disease because of its potential to produce lasting remission without the need for long-term drug or hormone replacement therapy. The authors evaluated the current role of pure endoscopic endonasal pituitary surgery in the treatment of Cushing disease. Methods: Twenty-five patients underwent pure endoscopic surgery for confirmed Cushing disease. Thirteen patients had microadenomas and seven had macroadenomas; magnetic resonance images obtained in five patients were only suspicious or nondiagnostic, and thus they underwent inferior petrosal sinus sampling. Two patients had evidence of cavernous sinus involvement. Final histological results were consistent with adrenocorticotropin hormone (ACTH)–secreting adenoma in 20 patients. Results: Twenty patients (80%) had clinical remission and laboratory confirmation of hypocortisolemia (serum cortisol < 100 nmol/L requiring substitution therapy), suppression to low-dose dexamethasone, and normal 24-hour urinary free cortisol. The median follow-up period was 17 months (range 3–32 months). There was no recurrence at the time of the last follow-up. Three patients presented with new anterior pituitary deficiency, but no one had permanent diabetes insipidus. In one patient a cerebrospinal fluid leak developed but later resolved following lumbar drainage. Treatment failure was attributable to involvement of the cavernous sinus in two patients, incomplete tumor removal in one, negative exploration in one, and nodular corticotroph hyperplasia of the pituitary gland in one. Conclusions: Early results indicated that endoscopic endonasal surgery is a safe and effective treatment for ACTH-producing adenomas. The rate of remission in this study is comparable to those in previous series, and the rate of major postoperative complications is extremely low. Further studies with a larger number of patients and longer follow-ups are required to determine whether this more minimally invasive pure endoscopic approach should become the standard of care for the surgical treatment of Cushing disease. Keywords: adrenocorticotropin hormone–secreting adenoma; Cushing disease; endoscopic surgery; minimally invasive surgery; outcome; transsphenoidal approach. From The Journal of Neurosurgery, September 2007 Volume 23, Number 3 at http://thejns.org/toc/foc/23/3?cookieSet=1 |
10/31/2007 | |
Cushing disease: use of perioperative serum cortisol measurements in early determination of success following pituitary surgery |
Download Cushing disease: use of perioperative serum cortisol measurements in early determination of success following pituitary surgeryArmand Krikorian, M.D., Dima Abdelmannan, M.D., Warren R Selman, M.D., and Baha M Arafah, M.D. Abbreviations used in this paper: ACTH = adrenocorticotropic hormone; HPA = hypothalamic-pituitary-adrenal. Address correspondence to: Baha M. Arafah, M.D., Division of Endocrinology, University Hospitals/Case Medical Center, 11100 Euclid Avenue, Cleveland, Ohio 44106. email: baha.arafah@case.edu. Abstract: Despite many recent advances, management of cases of Cushing disease continues to be challenging. After complete resection of ACTH-secreting adenomas, patients develop transient ACTH deficiency requiring glucocorticoid replacement for several months. The current recommendation by many centers, including ours, for patients with ACTH-secreting adenomas is to withhold glucocorticoid therapy during and immediately after adenomectomy until there is clinical or biochemical evidence of ACTH deficiency. A serum cortisol level of less than 2 ?g/dl within the first 48 hours after adenomectomy is a reliable biochemical marker of ACTH deficiency and is associated with clinical remission of Cushing disease. Higher serum cortisol levels in the immediate postoperative period should be interpreted with caution. The decision to immediately reexplore the sella turcica should be individualized, taking into account the findings at surgery, the histopathological findings, and the changes in serum cortisol levels as well as the patient's wishes and concerns. Optimal diagnosis and therapy for patients with Cushing disease require thorough and close coordination and involvement of all members of the management team. Keywords: adenoma; cortisol; Cushing disease; Cushing syndrome; pituitary surgery. From The Journal of Neurosurgery, September 2007 Volume 23, Number 3 at http://thejns.org/toc/foc/23/3?cookieSet=1 |
10/31/2007 | |
Cyclic Cushing syndrome: definitions and treatment implications |
Download Cyclic Cushing syndrome: definitions and treatment implicationsMary Lee Vance, M.D. From The Journal of Neurosurgery, September 2007 Volume 23, Number 3 at http://thejns.org/toc/foc/23/3?cookieSet=1 |
10/31/2007 | |
Cyclic Cushing syndrome: definitions and treatment implications |
Download Cyclic Cushing syndrome: definitions and treatment implications(Response to Dr Vance's article, above) Dennis A. Velez, M.D., Marc R. Mayberg, M.D., and William H. Ludlam, M.D., Ph.D. Abbreviations used in this paper: ACTH = adrenocorticotropic hormone; CRH = corticotropin-releasing hormone; CS = Cushing syndrome; TSA = transsphenoidal adenomectomy; UFC = urinary free cortisol. Address correspondence to: Marc R. Mayberg, M.D., 550 17th Avenue, Suite 500, Seattle, Washington 98122. email: marc.mayberg@swedish.org. Abstract: Endogenous Cushing syndrome (CS) results from hypercortisolemia caused by excess adrenocorticotropic hormone production in a pituitary adenoma or ectopic tumor, or by an adrenal tumor that directly produces excess cortisol. The diagnosis can usually be ascertained with a reasonable degree of certainty based on clinical and laboratory findings of hypercortisolism. There are patients, however, in whom the production of excess cortisol exhibits a cyclic or intermittent pattern, and, as a result, the clinical symptoms may be quite complex and varied. In these patients the hypothalamic-pituitary-adrenal axis may be normal between cycles, and dexamethasone suppression testing may produce a paradoxical response. In the present article, the authors provide a definition of cyclic Cushing syndrome, review the causes and its potential pathophysiological mechanisms, and discuss the treatment options based on a review of the available literature. Keywords: cyclic Cushing disease; hypercortisolism; pituitary adenoma; adrenocorticotropic hormone. From The Journal of Neurosurgery, September 2007 Volume 23, Number 3 at http://thejns.org/toc/foc/23/3?cookieSet=1 |
10/31/2007 | |
Diagnosis and Management of Cushing Disease |
Diagnosis and Management of Cushing DiseaseWilliam T. Couldwell, M.D., Ph.D. From The Journal of Neurosurgery,September 2007 Volume 23, Number 3 at http://thejns.org/toc/foc/23/3?cookieSet=1 |
10/31/2007 |
|
Diagnostic approach to Cushing disease |
Download Diagnostic approach to Cushing diseaseBradley A. Gross, B.S., Stefan A. Mindea, M.D., Anthony J. Pick, M.D., James P. Chandler, M.D., and H. Hunt Batjer, M.D. Abbreviations used in this paper: ACTH = adrenocorticotropic hormone; CD = Cushing's disease; CRH = corticotropin-releasing hormone; EAS = ectopic ACTH secretion; IPSS = inferior petrosal sinus sampling; MR = magnetic resonance. Address correspondence to: Shivanand P. Lad, M.D., Ph.D., Stanford Hospital, Department of Neurosurgery, 300 Pasteur Drive Room R281 MC5327, Stanford, California 94305. email: nlad@stanford.edu. Abstract: Cushing's syndrome can present a complex problem of differential diagnosis. Of cases in which hypercortisolemia results from an adrenocorticotropic hormone (ACTH)–dependent process, approximately 80% are due to a pituitary adenoma (Cushing's disease [CD]), 10% are due to adrenal lesions, and the remaining 10% are secondary to ectopic ACTH secretion. For patients with CD, surgical removal of the pituitary adenoma is the treatment of choice. Thus, localization of the source of ACTH secretion is critical in guiding timely treatment decisions. Inferior petrosal sinus sampling (IPSS) is considered to be the gold standard for confirming the origin of ACTH secretion in patients with Cushing's syndrome. The authors present an overview of IPSS—both the technique and its interpretation—as well as a summary of recent studies. A number of other techniques are discussed including sampling from the cavernous sinus, the jugular vein, and multiple sites to aid the diagnosis and lateralization of ACTH-producing pituitary adenomas. Management is best undertaken by a comprehensive multidisciplinary team taking into account the results of all the biochemical and imaging studies available, to provide the best advice in patient treatment decisions. Keywords: Cushing's disease; Cushing's syndrome; diagnosis; inferior petrosal sinus sampling. From The Journal of Neurosurgery, September 2007 Volume 23, Number 3 at http://thejns.org/toc/foc/23/3?cookieSet=1 |
10/31/2007 | |
Evaluation and management of Cushing syndrome in cases of negative sellar magnetic resonance imaging |
Download Evaluation and management of Cushing syndrome in cases of negative sellar magnetic resonance imagingJay Jagannathan, M.D., Jason P. Sheehan, M.D., Ph.D., and John A. Jane Jr., M.D. Abbreviations used in this paper: ACTH = adrenocorticotropic hormone; CRH = corticotrophin-releasing hormone; CSF = cerebrospinal fluid; LINAC = linear accelerator; MR = magnetic resonance; SPGR = spoiled gradient recalled acquisition in the steady-state; UFC = urinary free cortisol. Address correspondence to: Jay Jagannathan, M.D., Department of Neurological Surgery, University of Virginia Health System, Charlottesville, Virginia 22908. email: jj5a@hscmail.mcc.virginia.edu. Abstract: The treatment of patients with Cushing disease and without magnetic resonance (MR) imaging evidence of Cushing disease (that is, negative MR imaging) is discussed in this paper. Magnetic resonance imaging is the diagnostic modality of choice in Cushing disease, but in up to 40% of these patients negative imaging can be caused by tumor-related factors and limitations in imaging techniques. In cases in which the MR imaging is negative, it is critical to make sure that the diagnosis of Cushing disease is correct. This can be accomplished by performing a complete laboratory and imaging workup, including dexamethasone suppression tests, imaging of the adrenal glands, and inferior petrosal sinus sampling when appropriate. If these evaluations suggest a pituitary source of the hypercortisolemia, then transsphenoidal surgery remains the treatment of choice. The authors favor the endoscopic approach because it gives a wider and more magnified view of the sella and allows inspection of the medial cavernous sinus walls. Radiosurgery is an effective treatment option in patients with persistent Cushing disease. When a target cannot be found on MR imaging, one can target the entire sellar region with radiosurgery. Keywords: Cushing disease; Gamma Knife; magnetic resonance imaging; outcome; pituitary; pseudocapsule; radiosurgery; surgery. From The Journal of Neurosurgery, September 2007 Volume 23, Number 3 at http://thejns.org/toc/foc/23/3?cookieSet=1 |
10/31/2007 | |
Medical management of Cushing disease |
Download Medical management of Cushing diseaseBradley A. Gross, B.S., Stefan A. Mindea, M.D., Anthony J. Pick, M.D., James P. Chandler, M.D., and H. Hunt Batjer, M.D. Abbreviation used in this paper: ACTH = adrenocorticotropic hormone. Address correspondence to: Bradley Gross, B.S., 244 East Pearson Street, No. 310, Chicago, Illinois 60611. email: b-gross@md.northwestern.edu. Abstract: Although transsphenoidal excision of the adrenocorticotropic hormone (ACTH)–producing neoplasm is often the treatment of choice in patients with Cushing disease, medical management is itself a useful preoperative temporizing measure, an option for long-term management in nonsurgical candidates, and an option for patients in whom surgery and/or radiotherapy have failed. Three pathophysiologically based approaches exist in the research literature—neuro-modulation to limit ACTH levels, adrenal enzyme inhibition, and glucocorticoid receptor antagonism. Unfortunately, the neuromodulatory approach involving agents such as bromocriptine, cyproheptadine, octreotide, and valproate has yielded only suboptimal results. Glucocorticoid receptor antagonism remains in its infancy but may overall be limited by side effects and a resultant increase in ACTH and cortisol levels. Adrenal enzyme inhibitors, however, offer substantial future promise in the management of Cushing disease but are limited by the potential need to use them indefinitely and by dose-tolerance effects. Although etomidate is a potential intravenous alternative for acute cortisol level control, ketoconazole has shown efficacy in the long-term treatment of patients with the disease. Metyrapone and/or aminoglutethimide can be added to ketoconazole if additional control is needed. If success is still not achieved, the potent adrenolytic agent often used for adrenocortical carcinomas, mitotane, is another alternative. Keywords: aminoglutethimide; Cushing disease; etomidate; ketoconazole; metyrapone; mitotane. From The Journal of Neurosurgery, September 2007 Volume 23, Number 3 at http://thejns.org/toc/foc/23/3?cookieSet=1 |
10/31/2007 |
|
National trends, complications, and outcomes following transsphenoidal surgery for Cushing's disease from 1993 to 2002 |
Download National trends, complications, and outcomes following transsphenoidal surgery for Cushing's disease from 1993 to 2002Chirag G. Patil, M.D., Shivanand P. Lad, M.D., Ph.D., Griffith R. Harsh, M.D., Edward R. Laws Jr., M.D., and Maxwell Boakye, M.D. Abbreviations used in this paper: ACTH = adrenocorticotropic hormone; AHRQ = Agency for Healthcare Research and Quality; CI = confidence interval; DI = diabetes insipidus; ICD-9 = International Classification of Diseases, 9th Revision; LOS = length of stay; NIS = Nationwide Inpatient Sample; OR = odds ratio; TSS = transsphenoidal surgery. Address correspondence to: Chirag G. Patil, M.D., Stanford Hospital, Department of Neurosurgery, 300 Pasteur Drive, Room R281 MC5327, Stanford, California 94305. email: chiragpatil@gmail.com. Object: Information about complications, patient outcomes, and mortality rate after transsphenoidal surgery (TSS) for Cushing's disease has been derived largely from single-institution series. In this study the authors report on inpatient death, morbidity, and outcomes following TSS for Cushing's disease on a national level. Methods: All patients in the Nationwide Inpatient Sample (NIS) database who had undergone transsphenoidal resection of a pituitary tumor for Cushing's disease between 1993 and 2002 were included in the study. The number of cases per year, length of stay (LOS), and rates of inpatient complications, death, and adverse outcomes (death or discharge to institution other than home) were abstracted. Univariate and multivariate analyses were performed to determine the effects of patient and hospital characteristics on outcome measures. Results: According to the NIS, there were an estimated 3525 cases of TSS for Cushing's disease in the US between 1993 and 2002. During this period, there was a trend toward a small increase in the number of TSSs for Cushing's disease. The in-hospital mortality rate was 0.7%, and the complication rate was 42.1%. Diabetes insipidus (15%), fluid and electrolyte abnormalities (12.5%), and neurological deficits (5.6%) were the most common complications reported. Multivariate analysis showed that complications were more likely in patients with pre-operative comorbidities. Patients older than 64 years were much more likely to have an adverse outcome (odds ratio [OR] 20.8) and a prolonged hospital stay (OR 2.2). Women were less likely than men to have an adverse outcome (OR 0.3). A single postoperative complication increased the mean LOS by 3 days, more than tripled the odds of an adverse outcome, and increased the hospital charges by more than US $7000. Conclusions: The authors provided a national perspective on trends, inpatient complications, and outcomes after TSS for Cushing's disease in the US. Postoperative complications had a significantly negative effect on LOS, adverse outcome, and resource utilization. Advanced age and multiple preoperative comorbidities were identified as important risk factors, and their effects on patient outcomes were quantified. Keywords: complication; Cushing's disease; national database; outcome; pituitary tumor; transsphenoidal surgery. From The Journal of Neurosurgery, September 2007 Volume 23, Number 3 at http://thejns.org/toc/foc/23/3?cookieSet=1 |
10/31/2007 | |
Nelson syndrome: comprehensive review of pathophysiology, diagnosis, and management |
Download Nelson syndrome: comprehensive review of pathophysiology, diagnosis, and managementMagdalena J. Banasiak, M.D. and Ali R. Malek, M.D. Abbreviations used in this paper: ACTH = adrenocorticotropic hormone; CD = Cushing disease; CRH = corticotropin-releasing hormone; CT = computed tomography; GH = growth hormone; MR = magnetic resonance; MSH = melanocyte-stimulating hormone; NS = Nelson syndrome; TBA = total bilateral adrenalectomy; TSH = thyroid-stimulating hormone. Address correspondence to: Ali R. Malek, M.D., Department of Neurosurgery, University of South Florida, 4 Columbia Drive, Suite 730, Tampa, Florida 33606. email: amalek@health.usf.edu. Abstract: Nelson syndrome (NS) is a rare clinical manifestation of an enlarging pituitary adenoma that can occur following bilateral adrenal gland removal performed for the treatment of Cushing disease. It is characterized by excess adreno-corticotropin secretion and hyperpigmentation of the skin and mucus membranes. The authors present a comprehensive review of the pathophysiology, diagnosis, and management of NS. Corticotroph adenomas in NS remain challenging tumors that can lead to significant rates of morbidity and mortality. A better understanding of the natural history of NS, advances in neurophysiology and neuroimaging, and growing experience with surgical intervention and radiation have expanded the repertoire of treatments. Currently available treatments include surgical, radiation, and medical therapy. Although the primary treatment for each tumor type may vary, it is important to consider all of the available options and select tthe one that is most appropriate for the individual case, particularly in cases of lesions resistant to intervention. Keywords: adrenalectomy; adrenocorticotropic hormone; hyperpigmentation; Nelson syndrome; pituitary adenoma. From The Journal of Neurosurgery, September 2007 Volume 23, Number 3 at http://thejns.org/toc/foc/23/3?cookieSet=1 |
10/31/2007 | |
Nelson syndrome: historical perspectives and current concepts |
Download Nelson syndrome: historical perspectives and current conceptsMark Hornyak, M.D., Martin H. Weiss, M.D., Don H. Nelson, M.D., and William T. Couldwell, M.D., Ph.D. Abbreviations used in this paper: ACTH = adrenocorticotropic hormone; MR = magnetic resonance. Address reprint requests to: William T. Couldwell, M.D., Ph.D., Department of Neurosurgery, University of Utah, 175 North Medical Drive East, Salt Lake City, Utah 84132. email: neurop-ub@hsc.utah.edu. Abstract: The appearance of an adrenocorticotropic hormone (ACTH)–producing tumor after bilateral adrenalectomy for Cushing disease was first described by Nelson in 1958. The syndrome that now bears his name was characterized by hyperpigmentation, a sellar mass, and increased plasma ACTH levels. The treatment of Cushing disease has changed drastically since the 1950s, when the choice was adrenalectomy. Thus, the occurrence, diagnosis, and treatment of Nelson syndrome have changed as well. In the modern era of high-resolution neuroimaging, transsphenoidal microneu-rosurgery, and stereotactic radiosurgery, Nelson syndrome has become a rare entity. The authors describe the history of the diagnosis and treatment of Nelson syndrome. In light of the changes described, the authors believe this disease must be reevaluated in the contemporary era and a modern paradigm adopted. Keywords: Cushing disease; Cushing syndrome; Nelson syndrome; neurosurgery history. From The Journal of Neurosurgery, September 2007 Volume 23, Number 3 at http://thejns.org/toc/foc/23/3?cookieSet=1 |
10/31/2007 | |
The role of inferior petrosal sinus sampling in the diagnostic localization of Cushing's disease |
Download The role of inferior petrosal sinus sampling in the diagnostic localization of Cushing's diseaseShivanand P. Lad, M.D., Ph.D., Chirag G. Patil, M.D., Edward R. Laws Jr., M.D., and Laurence Katznelson, M.D. Abbreviations used in this paper: ACTH = adrenocorticotropic hormone; CD = Cushing's disease; CRH = corticotropin-releasing hormone; EAS = ectopic ACTH secretion; IPSS = inferior petrosal sinus sampling; MR = magnetic resonance. Address correspondence to: Shivanand P. Lad, M.D., Ph.D., Stanford Hospital, Department of Neurosurgery, 300 Pasteur Drive Room R281 MC5327, Stanford, California 94305. email: nlad@stanford.edu. Abstract: Cushing's syndrome can present a complex problem of differential diagnosis. Of cases in which hypercortisolemia results from an adrenocorticotropic hormone (ACTH)–dependent process, approximately 80% are due to a pituitary adenoma (Cushing's disease [CD]), 10% are due to adrenal lesions, and the remaining 10% are secondary to ectopic ACTH secretion. For patients with CD, surgical removal of the pituitary adenoma is the treatment of choice. Thus, localization of the source of ACTH secretion is critical in guiding timely treatment decisions. Inferior petrosal sinus sampling (IPSS) is considered to be the gold standard for confirming the origin of ACTH secretion in patients with Cushing's syndrome. The authors present an overview of IPSS—both the technique and its interpretation—as well as a summary of recent studies. A number of other techniques are discussed including sampling from the cavernous sinus, the jugular vein, and multiple sites to aid the diagnosis and lateralization of ACTH-producing pituitary adenomas. Management is best undertaken by a comprehensive multidisciplinary team taking into account the results of all the biochemical and imaging studies available, to provide the best advice in patient treatment decisions. Keywords: Cushing's disease; Cushing's syndrome; diagnosis; inferior petrosal sinus sampling. From The Journal of Neurosurgery, September 2007 Volume 23, Number 3 at http://thejns.org/toc/foc/23/3?cookieSet=1 |
10/31/2007 | |
Transsphenoidal surgery for Cushing's disease: a review of success rates, remission predictors, management of failed surgery, and Nelson's Syndrome |
Download Transsphenoidal surgery for Cushing's disease: a review of success rates, remission predictors, management of failed surgery, and Nelson's SyndromeDaniel F. Kelly, M.D. Abbreviations used in this paper: ACTH = adrenocorticotropic hormone; MR = magnetic resonance. Address correspondence to: Daniel F. Kelly, M.D., John Wayne Cancer Institute at Saint John's Health Center, 2200 Santa Monica Blvd, Santa Monica Boulevard, California 90404. email: kellyd@jwci.org. Abstract: Cushing's disease is a serious endocrinopathy that, if left untreated, is associated with significant morbidity and mortality rates. After diagnostic confirmation of Cushing's disease has been made, transsphenoidal adenomectomy is the treatment of choice. When a transsphenoidal adenomectomy is performed at experienced transsphenoidal surgery centers, long-term remission rates average 80% overall, surgical morbidity is low, and the mortality rate is typically less than 1%. In patients with well-defined noninvasive microadenomas, the long-term remission rate averages 90%. For patients in whom primary surgery fails, treatment options such as bilateral adrenalectomy, stereotactic radiotherapy or radiosurgery, total hypophysectomy, or adrenolytic medical therapy need to be carefully considered, ideally in a multidisciplinary setting. The management of Nelson's Syndrome often requires both transsphenoidal surgery and radio-therapy to gain disease control. Keywords: adrenocorticotropic hormone; cortisol; Cushing's disease; Nelson's Syndrome; remission; transsphenoidal surgery. From The Journal of Neurosurgery, September 2007 Volume 23, Number 3 at http://thejns.org/toc/foc/23/3?cookieSet=1 |
10/31/2007 | |
Treatment options for Cushing disease after unsuccessful transsphenoidal surgery |
Treatment options for Cushing disease after unsuccessful transsphenoidal surgeryJames K. Liu, M.D., Maria Fleseriu, M.D., Johnny B. Delashaw Jr., M.D., Ivan S. Ciric, M.D., William T. Couldwell, M.D., and Ph.D. Abbreviations used in this paper: ACTH = adrenocorticotropic hormone; CRH = corticotropin-releasing hormone; GABA = y-aminobutyric acid; GI = gastrointestinal; MR = magnetic resonance; SRS = stereotactic radiosurgery. Address correspondence to: James K. Liu, M.D., Division of Neurosurgery, Evanston Northwestern Healthcare, 2650 Ridge Avenue, Evanston, Illinois 60201. email: jliu@enh.org. Abstract: Cushing disease is considered an aggressive pituitary endocrinopathy because of the devastating effects from untreated hypercortisolemia. Although they are histologically benign, these adrenocorticotropic hormone (ACTH)-secreting pituitary tumors are associated with significant morbidity and premature death. Currently, transsphenoidal surgery is the primary treatment of Cushing disease associated with an ACTH-secreting pituitary tumor, resulting in remission rates ranging from about 50 to 90%. Some patients, however, will not achieve sustained remission after transsphenoidal surgery and can exhibit persistent or recurrent Cushing disease that requires multimodal treatment to achieve remission. In these patients, options for treatment include repeat transsphenoidal resection, radiation therapy (including conventional fractionated radiation therapy and stereotactic radiosurgery), and medical therapy. Despite undergoing multiple treatment modalities, some patients may ultimately require bilateral adrenalectomy for definitive treatment to eliminate hypercortisolemia associated with Cushing disease. In this article, the authors review the treatment options for patients who have persistent or recurrent Cushing disease after unsuccessful transsphenoidal surgery. The indications, current results reported in the literature, and complications of each treatment modality are discussed. Keywords: adrenalectomy; Cushing disease; pituitary adenoma; stereotactic radiosurgery; transsphenoidal surgery. From The Journal of Neurosurgery, September 2007 Volume 23, Number 3 at http://thejns.org/toc/foc/23/3?cookieSet=1 |
10/31/2007 |
|
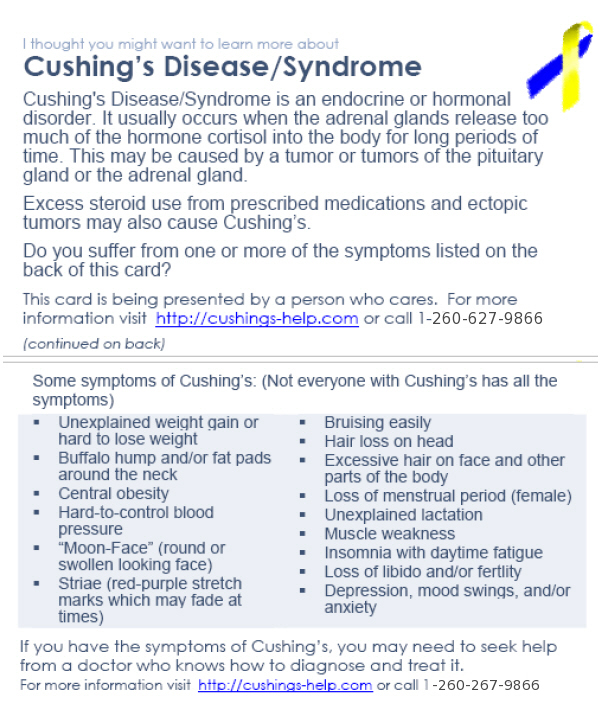
Spread The Word! Cushing's Pocket Reference |
Robin Writes:This has been a concern of mine for some time. Your post spurred me on to do something I've been meaning to do. I've designed something you can print that will fit on the business cards you can buy just about anywhere (Wal-mart included). You can also print on stiff paper and cut with a paper cutter or scissors. I've done a front and a back.
Here are the links:
• Front: This card is being presented by a person who cares.
|
9/29/2007 |
|
Cushings Help Organization, Inc. Printable Brochure |
Download Cushings Help Organization, Inc. Printable BrochureCushing's brochures that are sent out with the Cushing's Awareness Wristbands. Cushing's brochures that are sent out with the Cushing's Awareness Wristbands. Print them on special tri-fold brochure paper for the best effect. I update these after each meeting, when I have new pictures, so if you print them out, check back now and then for the latest copy. Newest version includes the new podcasts, voice chats / Internet Talk Radio and has a Columbus, OH picture |
Updated 1/09/2008 |
|
The Senate Resolution 127 (2007) PDF file |
Download The Senate Resolution 127 (2007) PDF fileCushing's Awareness Day! April 8, 2007 |
4/2/2007 |
|
Nutrition for Cushing's Patients |
Download Nutrition for Cushing's PatientsFrom the NIH (National Institutes of Health) |
10/31/2006 |
|
Cyclical Cushing's |
Download Cyclical Cushing'sYoung Sam's clinical results. She was born with cyclical adrenal Cushing's. |
10/31/2004 |
|
Podcast / Audio |
Pituitary Tumor(Podcast audio version) |
Dr. Salvatori discusses pituitary tumorsDr. Roberto Salvatori (MaryO's endo) Podcast |
10/10/2007 |
Real Player / Windows Media(TM) Video File |
Pituitary Cushing's(Real Player / Windows Media(TM) Video File version [16 MB]) |
Download Pituitary Cushing'sKate and Dr. Ted Friedman on National Geographic TV were featured on the National Geographic channel. The show, called the Science of Obesity, has a segment on Cushing's syndrome. Today, 127 million adult Americans are considered overweight, but few reach the extreme proportions of the exceptionally obese. What are the physical stresses of weighing more than 500 pounds and what steps can reverse it? NGC provides an understanding of what happens inside the bodies of these massive people & why a person can pack on hundreds more pounds than those with typical weight challenges. The show explores the genetics behind weight gain & medical advances available to help prevent it. I hope that all of you can watch this. Please consider contacting your local media about doing your story! There is still much work to do to increase Cushing's awareness. |
9/19/2007 |
Word |
Dear Senator... |
Download Dear Senator...Contact your Senator or Representative Print out a sample letter to send to your congress person or senator or download it in Word format. This will help pass Cushing's Awareness Day for another year |
3/15/2007 |
HOME | Sitemap | Adrenal Crisis! | Abbreviations | Glossary | Forums | Donate | Bios | Add Your Bio | Add Your Doctor
No forms of advertising are used on Cushings-Help.com.
All site features are available free of charge. But donations are gratefully accepted!
All site features are available free of charge. But donations are gratefully accepted!